Understanding postpartum nutrient depletion, the symptoms nobody warns you about, and why your prenatal vitamin might not be enough.
Five months postpartum, I stood in the Costco parking lot, a cart stuffed full of things I definitely did not come into Costco looking to purchase, a baby covered in the most epic blowout ever, and I couldn’t remember where I’d parked my car.
I had only been inside for maybe 30 minutes. Carrying my screaming baby, covered in poop, trying to push a cart… and my brain just couldn’t retrieve the information.
This wasn’t the first time. I had started taking pictures of where I parked because I couldn’t trust my memory anymore.
I felt like I was losing my mind.
The postpartum brain fog was constant. My brain felt thick and heavy and like I was viewing the world through dark sunglasses.
I had headaches. It constantly felt like there was a thick band surrounding my skull, squeezing it tight. A vice grip.
Once again, I thought something was seriously wrong with me.
But I told myself it was normal, it had to just be new mom stuff and something everyone experienced and just didn’t talk about. I was probably just tired. Everyone’s tired after having a baby, right?
Medical Disclaimer: This information is for educational purposes only and is not medical advice. Always consult a qualified healthcare provider for personalized guidance.
Partnership Disclosure: This post is sponsored by Needed, a brand I genuinely recommend to my community and use personally.
The Moment It All Clicked — What is Postpartum Depletion?
Not too long after this Costco event, I was doom-scrolling Instagram at 4am after a diaper change and during a nursing session. A post about postpartum nutrient depletion stopped me cold. It said something along the lines of this:
“Pregnancy doesn’t just deplete your nutrient stores. Postpartum can deplete you MORE. Breastfeeding pulls calcium from your bones, you lose zinc, magnesium, B vitamins, and iron – all while you’re running on no sleep and trying to feed another human from your body. And it takes YEARS to rebuild those stores if you’re not actively replenishing them.”
Um. WHAT?!
As I sat there in the dark, a precious baby in my arms, I felt it all click into place.
I wasn’t losing my mind. I was depleted.
The Prenatal Vitamin Mistake That Made Everything Worse
Here’s the annoying part: I’d taken a high-quality prenatal religiously throughout my entire pregnancy. It had methylated B vitamins, high levels of choline, impeccable ingredients sourcing, you know, the works.
Then I had a baby and… stopped???
I don’t even remember making the decision. I must have just run out, and I didn’t reorder. I was breastfeeding, exhausted, barely keeping us both alive. A multivitamin felt like one more thing I didn’t have the bandwidth for.
I didn’t know I’d just made one of the worst postpartum decisions possible.
Postpartum Depletion Symptoms: What the Research Actually Says
I started researching, and what I found was both validating and infuriating.
Pregnancy takes an estimated 1000mg of iron from maternal stores.[1] Breastfeeding pulls 200-300mg of calcium from your bones daily.[2] Exclusive breastfeeding increases zinc requirements by 50%.[3]
Choline—critical for brain function and mood regulation—is depleted during pregnancy and lactation. Over 90% of pregnant and postpartum women don’t get enough.[4]
Magnesium deficiency causes headaches, muscle tension, and impacts sleep.[6] Sound familiar?
The vice around my head? Probably magnesium.
The memory lapses? Could be iron, B12, or choline.
And here’s what shocked me: it can take 2-3 years to fully replenish nutrient stores after pregnancy and breastfeeding.[8] That’s IF you’re actively supplementing with quality nutrients.
If you’re not? Many women never fully recover before their next pregnancy. Each baby compounds the maternal depletion.[9]
Why Most Prenatal Vitamins Don’t Address Postpartum Depletion and Aren’t Enough
Once I understood depletion, I started evaluating prenatal vitamin labels differently.
Most prenatal vitamins are designed to meet minimum requirements during pregnancy. They’re not formulated to rebuild depleted nutrient stores or support the intense nutritional demands of breastfeeding and postpartum recovery.
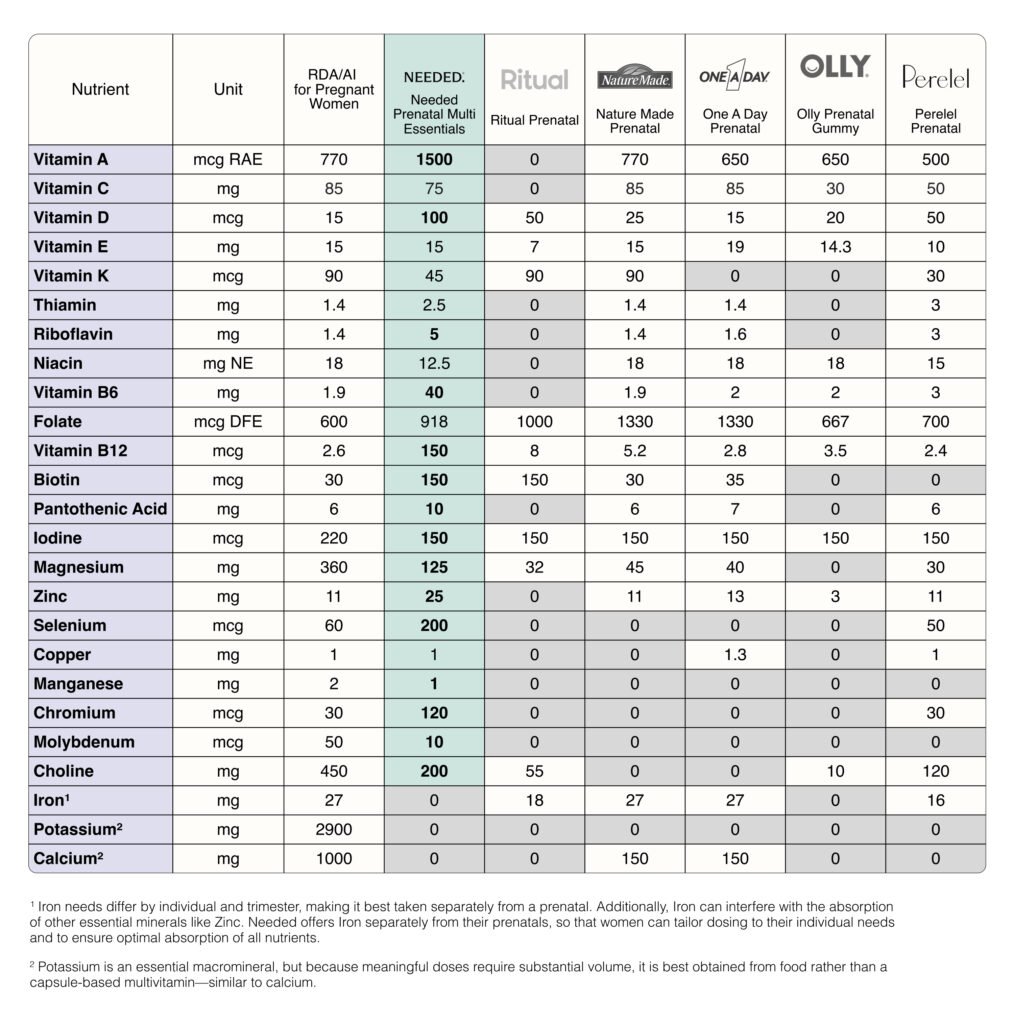
Here’s what I found when I compared prenatal vitamins:
Choline Content in Prenatal Vitamins
Most prenatal vitamins contain 50mg of choline or less. Some have zero choline. The research shows pregnant women need 450mg daily, breastfeeding women need 550mg.[10] That’s a massive gap.
Types of Iron in Prenatal Vitamins
Most prenatal vitamins use ferrous sulfate because it’s cheap. However, it can cause constipation in up to 50% of users and has lower absorption than other forms.[12] Not ideal when you’re already postpartum and/or dealing with hemorrhoids. Iron bisglycinate is a gentler, better-absorbed alternative and should only be used if lab values show a deficiency/low level.
Folate vs. Folic Acid: What’s the Difference
Up to 60% of people have a genetic variation (MTHFR) that makes it harder to convert synthetic folic acid into the active folate form their body can use.[13] Yet most prenatal vitamins still use folic acid instead of methylfolate.
On paper, standard prenatal vitamins look complete. In practice, they’re designed for bare minimum maintenance during pregnancy, and not postpartum depletion recovery.
The Best Prenatal for Beating Postpartum Depletion: What I Switched To
When I started looking for a prenatal that actually addressed depletion, I had specific requirements:
- Therapeutic nutrient doses, not token amounts
- Bioavailable vitamin and mineral forms for better absorption
- Formulated for the full maternal journey: preconception, pregnancy, AND postpartum
I chose Needed Prenatal Multi after weeks of comparing labels, and here’s what stood out:
400mg of choline. Not 50mg. Not zero. Actual meaningful amounts based on what research shows breastfeeding women need.
200mg of magnesium. Enough to actually address deficiency, not just check a box. I take an additional Magnesium supplement daily.
Separate iron supplementation with iron bisglycinate. Needed offers their iron separately (13.5mg per capsule) so you can adjust your dose based on your needs—2 capsules gives you the 27mg recommended during pregnancy. The iron bisglycinate form is gentler on your stomach and better absorbed than the ferrous sulfate found in most prenatals.
Methylated folate. The bioavailable form your body can actually use, rather than synthetic folic acid, which needs to be converted first—and that conversion doesn’t always happen or happen efficiently.
Designed for postpartum recovery. Most prenatal vitamins assume you stop supplementing after pregnancy. Needed’s formulation recognizes that postpartum and breastfeeding are when your body needs the MOST nutritional support.
It wasn’t the cheapest prenatal vitamin option. But after experiencing severe postpartum depletion and what I’d been through, I wasn’t taking chances with my health.
If you want to try Needed for yourself, I have an exclusive discount: 25% off new subscriptions through February 1st, 2026. Just use my link HERE and the discount applies automatically at checkout. Quality prenatal nutrition isn’t cheap, but after experiencing severe depletion, it became non-negotiable for me.
My Second Postpartum: How Proper Nutrition Changed Everything
I started taking Needed prenatal vitamins about six months before we tried for baby #2 (I was still nursing baby #1). I took it throughout my pregnancy, and I kept taking it postpartum while breastfeeding.
My second postpartum experience was completely different from my first. Like NIGHT AND DAY different.
No postpartum brain fog. No crushing headaches. No unwanted thoughts that made me feel like I was losing my mind. I was tired—of course I was tired, I had a toddler and a newborn—but I wasn’t nutritionally depleted.
There’s a crucial difference between normal postpartum tiredness and nutrient depletion, and I finally understood what that difference felt like.
I Am Still Taking Prenatal Vitamins 26 Months Postpartum: Here’s Why
I stopped breastfeeding months ago. My second baby is over two years old now.
And I’m STILL taking my prenatal vitamin.
Some people may think it’s overkill. And think, “But, you’re not even pregnant.”
Correct. But I don’t want to START my next pregnancy already running on empty like I did the first time.
Research shows it takes years to rebuild nutrient stores. I’m 26 months postpartum and just now feeling like my body is fully mine again. When we decide to try for baby #3, I want full reserves. I want to go into that pregnancy strong, not already depleted.
I’ve learned from experience, and I don’t ever want to feel that way again.
How to Choose the Best Prenatal Vitamin for Depletion Recovery
Whether you choose Needed or another high-quality prenatal, here’s what actually matters for addressing postpartum nutritional depletion:
Essential Nutrients to Look For:
Choline content: If it’s under 200mg, it’s not addressing postpartum and breastfeeding needs. Period.
Magnesium dose: Under 200mg won’t address deficiency. Look for 200mg+. I take an additional magnesium supplement.
Iron form: Ferrous bisglycinate or ferrous fumarate are better absorbed and gentler than ferrous sulfate. (In addition to iron rich foods. I took this separately.)
Folate type: Methylfolate (5-MTHF), not synthetic folic acid, especially if you have MTHFR gene variants.
Postpartum formulation: Does the brand even acknowledge that postpartum exists? Or do they assume pregnancy ends at delivery?
Postpartum Depletion Symptoms: When to Get Your Levels Checked
If you’re postpartum and experiencing these symptoms, ask your healthcare provider to check your nutrient levels:
Common postpartum depletion symptoms:
If you’re postpartum and feeling:
- Brain fog or memory lapses (postpartum cognitive decline)
- Crushing fatigue beyond normal tiredness
- Headaches, especially that tight band sensation
- Unwanted thoughts
- Postpartum hair loss
- Difficulty concentrating
- Muscle weakness or cramps
- Mood changes beyond typical baby blues
Some Lab Tests You Could Request:
- Ferritin (actual iron stores, not just hemoglobin)
- Vitamin D (25-hydroxyvitamin D)
- Vitamin B12 (cobalamin)
- Magnesium (RBC magnesium is more accurate than serum magnesium)
- Zinc levels
The biggest lessons I’ve learned are to not stop taking your prenatal after you give birth, to keep taking it through breastfeeding and postpartum recovery (for at least a year, probably longer, if you’re breastfeeding).
Your body just performed a biological miracle. It needs real nutritional support to rebuild.
There is Nothing Wrong With You – You’re Experiencing Postpartum Nutrient Depletion
I’m not saying supplements fix everything. I learned to ask for and accept help. I worked on sleep when I could, I prioritized nutrition, I didn’t skip meals, I ate a high protein breakfast before drinking coffee, etc.
But proper nutrition gave me the baseline brain function to actually engage, to be present with my kids, to remember where I parked my dang car.
Postpartum depletion isn’t a personal failure. It’s a predictable physiological outcome when your body gives more nutrients than it’s supported with.
And it’s fixable with the right nutritional support.
I never want to stand in that parking lot again, confused and overwhelmed. I never want that vice-grip headache or those unwanted thoughts that come with severe nutrient depletion.
Next time—if there is a next time—I’m going in nutritionally prepared.
Ready to Support Your Body?
Whether you’re dealing with postpartum depletion, preparing for pregnancy, or just want to stop running on empty, Needed has you covered. Beyond their prenatal line, they offer targeted support for sleep, cognitive function, immune health, fertility health, mood, and overall women’s and men’s wellness.

Exclusive reader discount: Get 25% off new Needed subscriptions and 30% off plans through February 1st, 2026. Use my link HERE and the discount applies automatically at checkout.
After my experience with severe depletion—the brain fog, headaches, and unwanted thoughts—investing in quality nutrition became non-negotiable. I wish I’d started sooner.
You don’t have to hit rock bottom before you take your health seriously. Start now.
How Needed Compares to Other Prenatal Vitamins
References:
[1] Bothwell TH. Iron requirements in pregnancy and strategies to meet them. Am J Clin Nutr. 2000;72(1):257S-264S.
[2] Kovacs CS. Maternal mineral and bone metabolism during pregnancy, lactation, and post-weaning recovery. Physiol Rev. 2016;96(2):449-547.
[3] Donangelo CM, et al. Zinc intake and homeostasis during lactation in Brazilian women. Nutrition. 2005;21(8):762-8.
[4] Wallace TC, Fulgoni VL. Assessment of total choline intakes in the United States. J Am Coll Nutr. 2016;35(2):108-12.
[5] Poly C, et al. The relation of dietary choline to cognitive performance and white-matter hyperintensity in the Framingham Offspring Cohort. Am J Clin Nutr. 2011;94(6):1584-91.
[6] Kirkland AE, et al. The role of magnesium in neurological disorders. Nutrients. 2018;10(6):730.
[7] Roomruangwong C, et al. Lowered global arginine bioavailability, increased oxidative stress and lower zinc are hallmarks of perinatal anxiety disorders. J Affect Disord. 2017;223:49-58.
[8] Darnton-Hill I, Mkparu UC. Micronutrients in pregnancy in low- and middle-income countries. Nutrients. 2015;7(3):1744-68.
[9] King JC. Physiology of pregnancy and nutrient metabolism. Am J Clin Nutr. 2000;71(5):1218S-25S.
[10] Institute of Medicine. Dietary Reference Intakes for Thiamin, Riboflavin, Niacin, Vitamin B6, Folate, Vitamin B12, Pantothenic Acid, Biotin, and Choline. National Academy Press; 1998.
[11] Institute of Medicine. Dietary Reference Intakes for Calcium, Phosphorus, Magnesium, Vitamin D, and Fluoride. National Academy Press; 1997.
[12] Tolkien Z, et al. Ferrous sulfate supplementation causes significant gastrointestinal side-effects in adults. PLoS One. 2015;10(2):e0117383.
[13] Crider KS, et al. MTHFR 677C→T genotype is associated with folate and homocysteine concentrations. Am J Clin Nutr. 2011;93(6):1365-72.

